Michigan statewide emergency dispatch survey
December 2021

- This brief is the result of a partnership between the Center for Behavioral Health and Justice (CBHJ), the National Emergency Number Association, and the Association of Public-Safety Communications Officials.
- In 2021, the CBHJ administered an online survey (N=114) to Public Service Telecommunicators (PSTs) to understand the state's emergency dispatch system.
- Included here are the survey findings and recommendations to improve crisis response through dispatch.
Dispatch and behavioral health crisis lines
- 74% reported that their Public Safety Answering Point (PSAP) receives calls from crisis lines.
- Only 30% of respondents said they will refer callers to behavioral health crisis lines.
- 19 respondents shared concerns of liability for transferring calls to behavioral health crisis lines.
- Many PSTs reported they would benefit from more behavioral health training.
- Concerns of personal, PSAP, and emergency response system liabilities were shared by respondents.
- The risk of not properly identifying low-risk mental health calls was also a concern.
Utilizing Crisis Intervention Teams (CIT) trained police officers
- Only 14% of respondents send CIT-trained officers to crisis calls.
- Of those who have access to CIT-trained officers, only 23% reported "definitely having" enough officers.
- Some dispatch centers did not know about their local CIT program until years after implementation.

*No CIT-trained officers
Identifying and coding mental health calls in dispatch systems
- There was no clear consensus on prevalence of mental health-related calls coming to 911.
- 50% of respondents estimated that a quarter or less of all dispatch calls are mental health-related.
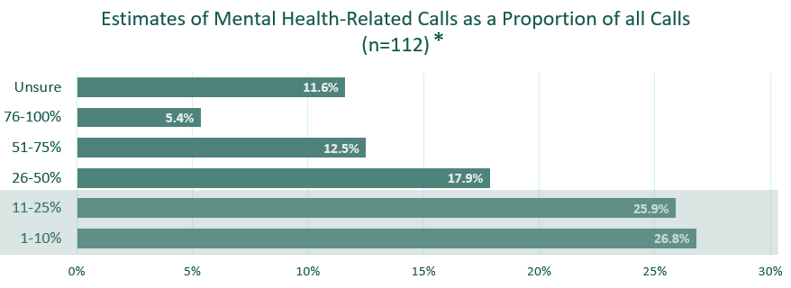
*Some respondents did not answer every survey question resulting in a smaller sample size.
Dispatch codes used for mental health crises
Mental Health (51.6%, n=47)
- Psychiatric
- Mental person or subject
- Insanity
- Emotionally disturbed
Welfare check (47.3%, n=43)
- Health & Safety
- Safety/wellbeing
- With or without EMS
Suicide (44.0%, n=40)
- Suicide in progress
- Suicidal person or subject
- Suicidal threat
- Suicidal thoughts or ideation
Other (16.5%, n=15)
- Disorderly
- Disturbance
- Suspicious
- Weapons
Substance use (12.1%, n=11)
- Overdose
- Drug
- Substance use or abuse
Medical (12.1%, n=11)
- Fire or police sick
- Ambulance
- Medical check
- Medic or medical
Assist (5.5%, n=5)
- Assist citizen or person
- Service for department
- Across various call scenarios, the most agreement from dispatchers was identifying a suicide call, followed by substance use, then mental health-related calls.
- There is no uniform coding of mental health calls across PSAPs.
- Out of 91 responses, including 31 unique counties*, only about half have specific call categories for mental health needs.
- New national dispatch standard from APCO recommends coding mental health crises.
Recommendations to improve crisis response collaboration with dispatch
- Behavioral health & criminal/legal collaborations should include dispatch to inform initiatives such as CIT, co-response, and mobile crisis units.
- Acknowledge dispatch concerns of liability and role perception when considering crisis system change.
- Code behavioral health crisis calls within 911 data, like the City of Detroit's Open Data Portal. Without coding these calls, we don't know how many mental health crises exist, or how they unfold.
- Fund pilot programs that embed crisis specialists, cross-train, and route calls from 911 to crisis lines.


