Expanding naloxone distribution in county jails
Recommended Practices for Implementation and Expansion of Jail-Based Naloxone Distribution Programs
June 2021
Compiled by: Nicole Hamameh, LMSW; Becca Newman, LLMSW; Rahni Cason, MA; Brad Ray, PhD; and Aliya Washington, BS
This toolkit is provided for informational and educational purposes only.
The Center for Behavioral Health and Justice (CBHJ) at the Wayne State University School of Social Work envisions communities in which research, data, and best practices are used by multiple partners to enhance the optimal wellbeing of individuals with mental illness and/or substance use disorders who come in contact with criminal-legal systems.
With over a decade of experience facilitating collaboration between criminal-legal partners and community-based treatment systems, the CBHJ currently serves as an external facilitator across Michigan. These engagements are focused on coordinating efforts to divert and deflect individuals from jail and prison through the implementation of best and innovative practices at every intercept of the criminal-legal continuum.
Acknowledgements
The CBHJ would like to thank our partners in the jails across Michigan who provided insight on their current naloxone distribution efforts, shared their expertise on the resources necessary to implement a naloxone distribution program, and identified barriers that often make it difficult to do so. This toolkit has been made possible by funding from the Michigan Department of Health and Human Services.
Toolkit origin and goals
An effective method for reducing opioid overdose in the community is providing naloxone upon release from custody in county jail. Naloxone is an FDA-approved medication that is nearly 100% effective in reversing the effects of an opioid overdose. It is often administered nasally under the common brand Narcan®, and available in an injectable form as well. While it is considered a prescription medication, there is a "standing order" in place in Michigan and many states across the nation which allows access to naloxone without an individual prescription.
Naloxone is safe, carries no risk for misuse, has no effect on an individual if opioids are absent, and still works for opioids even if other substances are present. The utility and safety of naloxone makes it a simple yet lifesaving tool for reducing overdoses involving opioids.
Providing barrier free naloxone for everyone released from jail is the primary objective of this toolkit.
With support from the Michigan Opioid Partnership and the Michigan Health Endowment Fund, the CBHJ has been working with county jails and treatment providers across the state of Michigan to intervene on behalf of individuals who are at the highest risk for overdose. Individuals with opioid use disorder (OUD) who have recently been released from jails or prisons experience an elevated risk for overdose, often with no path to engage in community-based treatment and no access to tools that can mitigate their immediate overdose risk.
The intended audience for this toolkit includes Sheriff's Offices, jail administrators, local health departments, and community-based organizations that are interested in implementing a naloxone distribution program or expanding current naloxone distribution efforts in their county jail. Access to naloxone for justice-involved individuals can save lives by reducing the incidence of fatal opioid overdose in the community.
Naloxone reverses opioid overdoses and saves lives.
For assistance implementing any of the strategies described in this toolkit or for more information about naloxone, please contact or email the CBHJ.
What is this life-saving medication?
Naloxone has been a standard medication used in emergency medicine for over 40 years. It can reverse an overdose from ANY opioid including heroin, prescription medications, and fentanyl.
To summarize research, not providing naloxone to jail detainees is contributing to rising rates of fatal overdose in the United States.
Opioid overdose occurs when an individual consumes higher levels of opioids than their body can handle, resulting in shut-down of the body's circulatory and respiratory systems. Signs of opioid overdose may include: unconsciousness, very small pupils, slow or shallow breathing, vomiting, inability to speak, a faint heartbeat, limp arms and legs, pale skin, or purple lips and fingernails. People experiencing an opioid overdose will die without the administration of naloxone.
Naloxone is the only antidote for an opioid overdose.
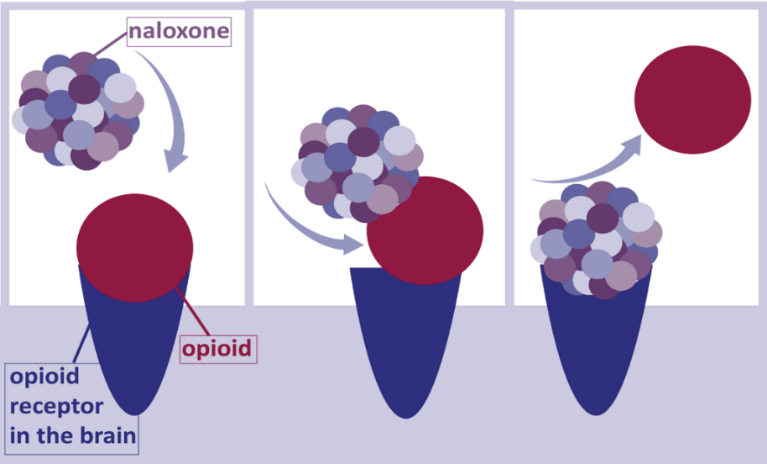
Naloxone works by knocking opioids off the receptors in the brain and replacing opioids with naloxone, to block opioids from re-attaching. Sometimes it can take multiple doses of naloxone to reverse an overdose, depending on the level of opioids present in the individual's brain at the time of administration. However, there is no opioid that cannot be reversed by administering enough naloxone, only .08% of reversals are unsuccessful. Individuals cannot become "immune" to naloxone, meaning it is still effective at reversing an opioid overdose for an individual who had a reversal previously.
Addressing safety and liability concerns
Naloxone is completely safe for anyone to carry and use when encountering an individual experiencing an overdose. Adverse effects are extremely rare when administering naloxone to someone experiencing an opioid overdose and naloxone will have no effect on an individual at all if they do not have opioids in their system. Naloxone does not make people violent about 2.1% of individuals experience agitation, and about 2.8% of individuals experience withdrawal symptoms when naloxone is administered. Naloxone cannot be abused.
There is no liability risk for providing naloxone to jail detainees. In the state of Michigan, there are several Public Acts in place to protect those who administer or distribute naloxone, including the "Good Samaritan" and related Public Acts1.
| MYTHS | FACTS |
|---|---|
| Having naloxone available encourages people to take more drugs. | Reversing an opioid overdose using naloxone gives that person a second chance at life and an opportunity to seek treatment if wanted. |
| Naloxone is another drug that can be abused. | Naloxone is safe and effective, and has no potential for abuse. In addition, naloxone cannot be taken before drug use to avoid an overdose. |
| I can only get naloxone if I have a prescription form a doctor. | Any person can purchase naloxone at a pharmacy with or without a prescription. However, this does not necessarily mean that every pharmacy will always stock naloxone, so we suggest calling ahead to make sure they have it on the shelf. |
| For more myths and facts about naloxone, fentanyl, and medications for opioid use disorder, visit the DOTS Project. | |
Building capacity to provide naloxone to all
Post-release opioid overdose mortality is the leading cause of preventable death among individuals exiting a correctional setting2. Overdose typically occurs within the first two weeks of release and is the leading cause of death among former inmates3-4.
The risk of overdose death is up to 130 times greater for an individual within two weeks following their release from incarceration than for someone without criminal/legal system involvement.
Supporting widespread distribution of naloxone providing access to everyone released from jail is the primary objective of this toolkit. The goal should be providing naloxone to as many people as possible with minimal time and effort required, reducing harm not just for opioid-involved individuals but for the community as a whole.
This toolkit describes several strategies to guide your facility in implementing a naloxone distribution program or expanding your current distribution efforts. When widespread distribution is not feasible, there are other lower impact strategies described in the following sections to guide distribution for specific populations or provide information about where individuals can access naloxone in the community following release.
Regardless of which strategies are selected, increasing awareness of and access to naloxone will help prevent fatal overdose and save lives in your community.
The CBHJ recommends developing a clear communication plan to delineate who is responsible for completing the various tasks of a naloxone distribution program. These tasks may include maintaining supply of naloxone kits, administering screening, provision of overdose prevention training, tracking participation, or arranging for distribution of naloxone kits. A sample communication plan can be downloaded here (.doc file).
Free naloxone for jails and community organizations
The Michigan Department of Health and Human Services has made it possible for local jails, law enforcement, and community organizations to request free nasal naloxone kits for distribution. To request a supply of naloxone kits, organizations should submit the request form and emailing the completed form to MDHHS-NalxneRqst@michigan.gov. If your agency is outside of Michigan, NEXT Distro offers kits and training to all, just select your state and find the agency closest to you.
Following submission of the order form, your organization can expect the naloxone kits to arrive within one to four weeks. If you do not receive your requested kits within this time frame, it is recommended that you send an email to MDHHS-NalxneRqst@michigan.gov to troubleshoot any problems related to your request.
| Submit order form to MDHHS by email | > | MDHHS processes order | > | Manufacturer ships naloxone kits | > | Naloxone kits arrive at facility in approximately one week |
Storage of naloxone
Naloxone should be stored at room temperature (between 59 and 86 degrees Fahrenheit) and in a dry area not exposed to direct sunlight. We recommend monitoring naloxone supplies to ensure you have enough for distribution and to prompt a new order when necessary. Tools such as a supply tracking spreadsheet can help monitor available supply. Additionally, expired naloxone is safe to use and can be just as effective as non-expired medication for up to 10 years. It should not be thrown away.
Expired naloxone is safe to use and can be just as effective as non-expired medication for up to 10 years. It should not be thrown away.
Identification of target population through screening
Many people leaving jail want naloxone not for themselves but because they are returning to communities where family members, friends, and neighbors use opioids and are at risk for overdose. The CBHJ recommends making naloxone available to all jail detainees, not just those who are at risk for opioid use or other behavioral health disorders.
The CBHJ recommends making naloxone available to all jail detainees, not just those who are at risk for opioid use or other behavioral health disorders.
Some jails prefer to identify a target population to receive naloxone at release but must first develop a process or standard for identifying these individuals. Participation in behavioral health programming, or identification as opioid-involved, or at risk of opioid use, are good indicators an individual should receive naloxone.
A self-report screening at booking or initial medical intake is an easy way to identify opioid-involved individuals. The Rapid Opioid Dependence Screen (RODS) is a validated tool that can be administered at booking and is very effective at identifying people who may be at risk for opioid use disorder. Any YES response to items 1a-1d on this assessment can be used to determine eligibility to receive naloxone at release. Some jails administer this assessment as a printed document that is filled out by hand; others have electronically embedded the assessment into their jail management system. The CBHJ recommends electronic collection of these types of assessments whenever possible.
Download the Rapid Opioid Dependence Screen (RODS)
Brief overdose prevention training
Naloxone is an inherently safe medication that can be used by anyone and requires very minimal training. Training can be as brief as providing a one-page document with the naloxone kit that is distributed, a somewhat more-involved video training, or an extensive overdose prevention class. For ease of management, the CBHJ recommends distribution of a one-page instructional sheet and/or showing a brief training video. In addition, the business card of a local harm reduction agency may be included as they typically offer naloxone trainings. Sample training videos and brief instructional guides can be accessed below.
Training Videos
Narcan® nasal spray training video
Instructional Guides
Opioid safety and how to use naloxone (ca.gov)
Jails may want to track who has received overdose prevention training to identify those who should receive a naloxone kit at release. A sample spreadsheet to track overdose prevention or naloxone training can be downloaded here (.xlsx file).
Strategies for naloxone distribution
- Overdose-reversal vending machine
High impact:

 A new approach to naloxone distribution in jails involves the use of vending machines. The machines are placed in jail lobbies, release areas, or other public spaces near a jail where released inmates could easily access naloxone. This strategy has been successfully implemented in Los Angeles County and other jails across the United States, and will be implemented in Michigan in the summer of 2021.
A new approach to naloxone distribution in jails involves the use of vending machines. The machines are placed in jail lobbies, release areas, or other public spaces near a jail where released inmates could easily access naloxone. This strategy has been successfully implemented in Los Angeles County and other jails across the United States, and will be implemented in Michigan in the summer of 2021. Each vending machine can hold up to 300 naloxone kits, which means the need to refill the machine will be very limited. In most cases, vending machines will be refilled by partners from your local health department or community mental health agency, eliminating the need for jail staff to manage distribution at all.
Los Angeles County, California
Los Angeles County Jail implemented an Overdose Education and Naloxone Distribution (OEND) program in June 2019 which provides overdose prevention and response video training and access to free naloxone for every individual who is released from the LA County Jail. During the first 9 months of 2020, more than 20,000 doses of naloxone were distributed through free self-serve vending machines located in the secure release area of the LA County Jail. Compared to other distribution methods, jail vending distribution achieved distribution at 2.5x the rate being achieved in the community during the same time period.
- Grab-and-go fishbowl
High impact:

 The release area "stopping point" is a prime location to place a fishbowl or other large container that holds multiple naloxone kits. The container should include a label that indicates the naloxone is free to take as individuals are being released. This strategy allows for easy viewing of the naloxone supply so your staff know when to refill the container or reorder additional kits. The CBHJ recommends identifying an individual or department that will be responsible for refilling the container and reordering additional supply of kits.
The release area "stopping point" is a prime location to place a fishbowl or other large container that holds multiple naloxone kits. The container should include a label that indicates the naloxone is free to take as individuals are being released. This strategy allows for easy viewing of the naloxone supply so your staff know when to refill the container or reorder additional kits. The CBHJ recommends identifying an individual or department that will be responsible for refilling the container and reordering additional supply of kits. - Placement in property box
 Automatic for all detainees
Automatic for all detaineesHigh impact:

Automatic placement in an individual's property box prior to release is one of the best ways to ensure that person will receive a naloxone kit when they leave your facility. The CBHJ recommends that a property officer or other responsible individual automatically puts a naloxone kit into each and every property box that comes through to be catalogued.
Target population only
Moderate impact:

Jails may prefer to determine eligibility to receive naloxone by an individual's participation in a specific program or for people who have been identified as being at-risk for opioid use disorder. When detainees are identified as eligible to receive naloxone, a property officer or other responsible individual puts a naloxone kit into that person's property box to receive at release.
Kent County, Michigan
By screening all jail detainees at booking, Kent County Correctional Facility is able to identify individuals who may be at risk for opioid use disorder to link them with recovery and overdose prevention resources. All individuals at risk for opioid use disorder receive an internal "O-alert" which notifies the behavioral health manager to automatically place a naloxone kit in their property box. Each naloxone kit also includes a business card for the Opioid Treatment Ecosystem Case Manager and for Red Project, a local harm reduction agency, as well as a flier that includes an array of local recovery and overdose prevention resources.
While targeted distribution is sometimes considered ideal by corrections agencies, it can be a complex process to approach distribution in this way. If a jail implements this targeted approach, it is imperative that roles and responsibilities of involved organizations are clearly identified. More information on this approach can be accessed in the Identification of a target population section.
- Referral to community-based naloxone distribution
Low impact:

Several community-based organizations provide free naloxone to anyone who requests it. Harm reduction agencies, local health departments, community mental health agencies, and other community-based organizations often provide free naloxone and overdose prevention training, among other supportive resources that may be useful for someone recently released from incarceration.
Making a direct referral to one of these types of organizations informs the person being referred about a specific location they can go to obtain naloxone, but also provides the specified organization with information about why this individual is requesting naloxone. The CBHJ recommends contacting local organizations prior to making referrals to confirm they are currently distributing naloxone.
Two of the largest harm reduction agencies in Michigan are The Red Project and Harm Reduction Michigan. In addition to naloxone distribution and overdose prevention training, these organizations provide safe syringe exchange services, peer recovery coaching, case management, and connection to other health resources. HarmRedcution.org is a national resource for harm reduction practices and overdose prevention. NEXT Distro is a national platform on which individuals would select their state to learn about pharmacies that carry naloxone, receive naloxone training, and even have naloxone mailed to the individual directly.
-
The Red Project (serves Allegan, Kent, Lake, Mason, Muskegon, Newaygo and Ottawa counties)
-
Harm Reduction Michigan (serves Emmett, Grand Traverse, Jackson, Kalkaska, Lake, Midland, Washtenaw, Wayne, and Wexford counties)
-
NEXT Distro is a national organization that provides free naloxone and training
Behavioral health services in Michigan are coordinated by local community mental health services programs. Contact information for your local community mental health organization can be accessed by selecting your county on the map located here.
Local health departments promote healthy communities, prevent outbreaks and disease, and help prepare for and respond to disasters and emergencies. Contact information for your local health department can be accessed by selecting your county on the map located here.
A sample referral form can be downloaded here (.docx file).
-
- Informational sign, brochure, or business card
Low impact:

Hanging informational signs and distributing flyers, brochures, or business cards to inmates with their property at release are also effective tools for widely sharing information on how to access naloxone following release. Distributed materials should be brief, but may include more information than would be included on a poster or sign. If not in the booking or release area, signage should be in a place of high-traffic where individuals will have time to read the information completely.
Materials should include some basic information about naloxone, including:
- Naloxone saves lives
- Naloxone is safe to use and is highly effective at reversing opioid overdose
- List the names and contact information for several community-based organizations or pharmacies where naloxone can be accessed for free
- Include information on how to access free naloxone online
A sample flier can be downloaded here (.docx file).
A sample business card can be downloaded here (.docx file).
- OpiRescue app
Low impact:

No matter where you're located, OpiSafe is a national online resource that both care providers and individuals can use.
Providers can access information on best prescribing practices and overdose prevention and can also be used as a data collection platform.
Individuals leaving jail can download the OpiRescue app from any phone to access resources in their community related to MOUD and overdose prevention, as well as step by step instructions on how to administer naloxone during an overdose event. Jails can facilitate access to this app by distributing business cards with a QR code that can be scanned for easy download.
Footnotes
- Michigan "Good Samaritan" Act (PA 307-308 of 2016), PA 39 of 2019, PA 311-314 of 2014; Good Samaritan Laws Across the U.S. ^Back
- Jourdey, 2019 ^Back
- Krinsky, C. S., Lathrop, S. L., Brown, P., & Nolte, K. B. (2009). Drugs, Detention, and Death: A Study of the Mortality of Recently Released Prisoners. The American Journal of Forensic Medicine and Pathology, 30(1), 69. https://doi.org/10.1097/PAF.0b013e3181873784 ^Back
- Binswanger, I. A. (2013). Mortality After Prison Release: Opioid Overdose and Other Causes of Death, Risk Factors, and Time Trends From 1999 to 2009. Annals of Internal Medicine, 159(9), 592. https://doi.org/10.7326/0003-4819-159-9-201311050-00005 ^Back
- Davidson, 2019 ^Back
