SAMHSA reduces barriers to new methadone patients in jail through crisis exceptions during the COVID-19 pandemic
Jails seeking to begin individuals on  methadone treatment for opioid use disorder (OUD) during the COVID-19 pandemic now have one less barrier to overcome. Under the crisis exceptions in place during the pandemic, the Substance Abuse and Mental Health Services Administration (SAMHSA) will allow Opioid Treatment Program (OTP) providers across the country to observe in-person physicals conducted by certain jail medical staff over telehealth for methadone inductions.
methadone treatment for opioid use disorder (OUD) during the COVID-19 pandemic now have one less barrier to overcome. Under the crisis exceptions in place during the pandemic, the Substance Abuse and Mental Health Services Administration (SAMHSA) will allow Opioid Treatment Program (OTP) providers across the country to observe in-person physicals conducted by certain jail medical staff over telehealth for methadone inductions.
Jails have been disproportionately impacted by both the COVID-19 pandemic and the opioid epidemic, and the crises have merged to form a "syndemic". More than 30 states have reported increases in opioid-related use and deaths since the pandemic began. In order to reduce traffic and limit the spread of COVID-19, many correctional facilities have temporarily restricted or suspended access to outside personnel, including OTP providers. Further, many courts have slowed or paused proceedings, significantly postponing release dates for those awaiting trial.
At the end of April, SAMHSA shared a FAQ document clarifying the crisis exceptions for behavioral health services during the COVID-19 pandemic. While OTP providers in any setting are temporarily exempt from providing in-person physicals to new patients on buprenorphine, the requirement of an in-person medical evaluation would remain in force for new patients on methadone. The Center for Behavioral Health and Justice (CBHJ) and Wayne State University's School of Social Work quickly identified the unique barriers this would present in jail settings.
The Opioid Treatment Ecosystem (OTE) initiative of the CBHJ supports county stakeholders in implementing or improving elements of Medication Assisted Treatment (MAT) practices in the criminal/legal system through the OTE Model (as seen below). In the beginning phase of the initiative, priority was placed on increasing access to Medications for Opioid Use Disorder (MOUD) in OTE county jails, as no treatment for opioid use disorder has stronger evidence supporting it than the three forms of FDA approved MOUD.
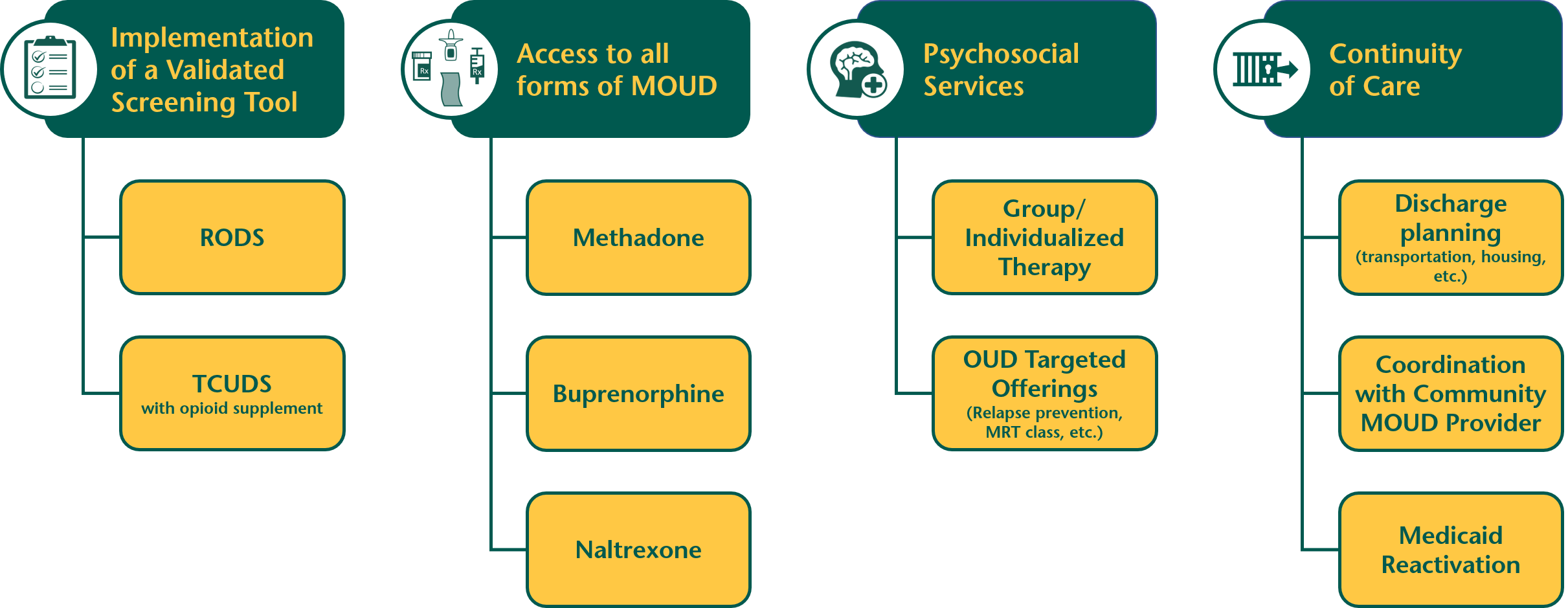
April's crisis exceptions alleviated COVID-19 related barriers to accessing buprenorphine in jail settings. While the groundbreaking work in several Michigan communities could resume in some ways, access to all three forms of FDA approved medications-including methadone-is a critical component of the OTE Model.
 School of Social Work Dean Sheryl Kubiak reached out to the Michigan Department of Health and Human Services and found an ally in Lisa Miller, the State Opioid Treatment Authority. Miller proposed the use of a telehealth connection, which would ensure that "all elements of the physical are conducted" while still allowing the provision of opioid treatment services in jail settings to move forward. In response, SAMHSA approved the use of a telehealth connection between the OTP provider and a jail-based nurse practitioner, physician assistant, or physician.
School of Social Work Dean Sheryl Kubiak reached out to the Michigan Department of Health and Human Services and found an ally in Lisa Miller, the State Opioid Treatment Authority. Miller proposed the use of a telehealth connection, which would ensure that "all elements of the physical are conducted" while still allowing the provision of opioid treatment services in jail settings to move forward. In response, SAMHSA approved the use of a telehealth connection between the OTP provider and a jail-based nurse practitioner, physician assistant, or physician.
Methadone, buprenorphine, and naltrexone are the FDA approved forms of MOUD, all of which are recommended for use in coordination with counseling and behavioral therapies. During the COVID-19 pandemic, allowing OTP physicians access to facilities may be the most thorough and cost-effective route for jails to begin methadone treatment for a new patient. However, any method for increasing access to all forms of MOUD and accurately identifying individuals with opioid use disorder are critical in addressing the opioid epidemic-a national crisis that has been heightened by the COVID-19 pandemic.
*Under the rubric of flexibilities allowed due to the COVID-19 crisis, jail-based nurse practitioners (NP), physician assistants (PA), and physicians may conduct the physical while being observed by the OTP medical director or physician though a telehealth connection. It is important to note that registered nurses (RN) and licensed practical nurses (LPN) cannot be used for this procedure. All elements and aspects of the physical should be fully documented in the patient's OTP record and signed by the OTP physician or medical director within 24 hours of induction.
About the Center for Behavioral Health and Justice: The Wayne State University School of Social Work Center for Behavioral Health envisions communities in which research, data, and best practices are used by multiple stakeholders to enhance the optimal well-being of individuals with mental illness and/or substance use disorders who come into contact with the criminal/legal system. Learn more